500+ Google Reviews
★★★★★ 4.9/5
4.9 out of 5
The best physios by far...
Truly outstanding experience...
...very friendly and welcoming.
...tons of experience.
...they have been amazing.
The foot and ankle is a complex area of anatomy. Our expert team of Physiotherapists have years of experiencing in assessing and treating foot and ankle conditions, and can help you quickly get back on your feet.
The complex biomechanical structure of the foot and ankle provides a stable base to bear our body weight and enable a range of functions including walking, running and adapting to uneven surfaces.
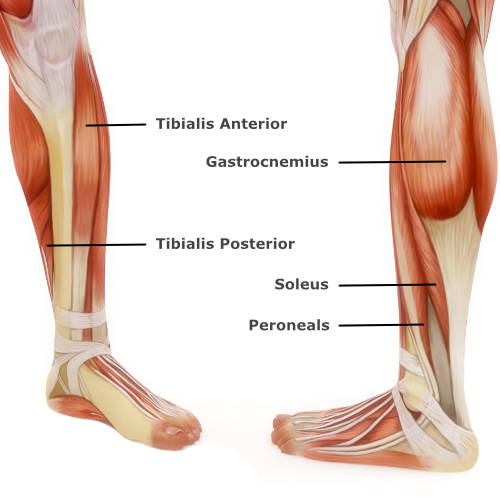
The ankle joint is the point where the tibia (shin bone) and fibula connect to the foot. It is supported by ligaments both on the inner aspect, and outer aspect of the ankle. Ligaments also exist between the tibia and fibula, near the ankle joint. This is called the syndesmosis. The main muscles acting on the ankle to provide movement, power and stability are the gastrocnemius, soleus, peroneal, tibialis anterior and tibialis posterior.
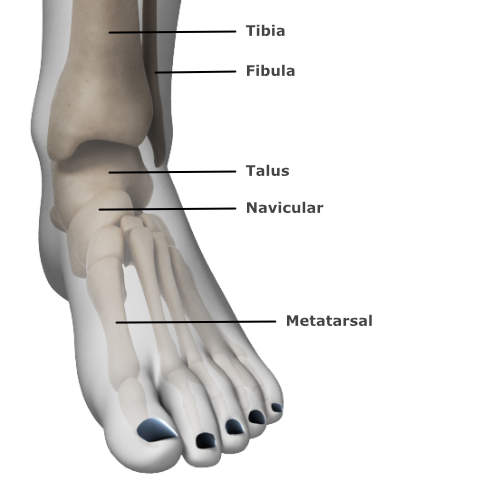
There are over 30 joints within the foot which consists of 26 bones. In clinic, the foot is often considered in three parts; the forefoot, the midfoot and the hindfoot.
The forefoot consists of metatarsals and the many ligaments that hold them together. A combination of small muscles (called intrinsics) and long tendons work together in the forefoot to create and control movement of the toes and aid propulsion.
The hind foot consists of the talus (ankle bone) and the calcaneous (the heel bone). The Achilles tendon inserts into the calcaneous and is responsible for moving the ankle up and down.
The midfoot contains five tarsal bones. The arch of the foot is formed by the tarsal bones and supported by the plantar-fascia and the tibialis posterior. It acts to absorb shock when we walk or run and adapts to facilitate balance on uneven surfaces.
The foot and ankle is a complex area of anatomy, consisting of 26 bones, more than 30 small joints and many muscles, tendons ligaments and nerves. Injuries can occur to any of these structures with varying severity.
The plantar-fascia is a thick band of tissue that runs from the heel to the big toe. It provides support to the medial arch of the foot.
Plantar-fasciitis is a common condition in which the plantar-fascia becomes irritated and sensitive at its attachment to the heel bone. This often presents as pain in the sole of the foot, particularly at the inner aspect of the heel. People with plantar-fasciitis can experience this pain when walking & running. It is often more severe first thing in the morning and on moving from static.
Risk factors for developing plantar-fasciitis include age, raised BMI, distance running, diabetes and sudden changes in activity levels.
The management of plantar-fasciitis include relative rest from the aggravating activities, a specific programme to stretch and progressively load the fascia and a graded return to activity. Adjunctive physiotherapy treatments including soft tissue treatment, acupuncture, taping & orthosis and shock wave therapy may also help.
Many cases of plantar-fasciitis resolve within six months of conservative treatment as described above. In more severe cases, where the pain is not improving as expected you may require a referral to a consultant to consider further treatment options.
A sprained ankle is a soft-tissue injury to the ligaments surrounding the ankle joint. It most commonly involves the ligaments on the outside of the ankle and occurs when you roll the ankle inwards. Ankle sprains are often graded out of 3 depending on how much soft-tissue is thought to be damaged.
Symptoms of a sprained ankle include pain, swelling, bruising, difficulty weight-bearing and ankle stiffness (most commonly pointing the toes or turning the foot inwards is restricted by pain). Also, as your ankle joint and ligaments provide your brain with a lot of feedback about where your ankle is in space, following an ankle sprain it is common to feel a bit unbalanced or as if your ankle may give way.
Most ankle sprains can be managed conservatively. Depending on the severity it may be appropriate to immobilise the ankle for a short period in a boot or brace to help it settle down and make weight-bearing easier. There is good evidence to suggest that early mobilisation and functional treatment produces better outcomes than immobilising the ankle for an extended period.
Most people who suffer from an ankle sprain make a complete recovery. Dependent on the grade of sprain the recovery may vary from 2 weeks to 6 months. In some more severe cases where the ankle is unstable, surgery may be appropriate although this is rare.
Physiotherapy following an ankle sprain may involve hands on treatment to restore range of movement, strengthening and balance exercises, taping or strapping, ultrasound and sports-specific rehabilitation in the later stages.
The Achilles tendon connects the muscles of the calf to the heel bone. Tendinopathy is the term used to describe an injury to the tendon and often occurs as a result of over-loading the tissues. Current research suggests that pain develops when the tendon regeneration process cannot keep up with the load being applied to the tendon. This often occurs due to sudden increases in activity levels, over-training and training error. Other factors including age, weight and smoking may also contribute to the development of Achilles tendon pain.
Symptoms of Achilles tendinopathy include pain and stiffness in the lower calf, the tendon and the heel. Pain and stiffness are often felt in the mornings and on moving from static positions. This usually settles with gentle movement. Walking and running can exacerbate the symptoms.
Achilles tendinopathy responds well to Physiotherapy. Pain and function generally improves with twelve weeks of rehabilitation and activity modification. A physiotherapist will be able to assess your symptoms and make recommendations regarding specific exercises to improve the load tolerance of the tendon. It may be necessary to reduce running or high impact activities in the initial phase your rehab; your physiotherapist will be able to advise you on alternate activities and a graded return to your sport.
Tibialis posterior (tib-post) tendinopathy is a common foot and ankle problem. It is an overuse injury to the tendon on the inner side of the ankle joint, just behind the ankle bone. It usually occurs as a result of repetitive activity or load, especially from high intensity activity such as running and jumping sports. Sometimes the tendon is injured as a result of a fall which can result in a tear. Obesity, diabetes and hypertension are all risk factors, as well as it being a more common injury in females and people aged over 40 years.
Symptoms of tib-post tendinopathy include pain around the inside of the ankle or arch of the foot. The tendon can be painful at its insertion into the navicular bone (a bone on the inside of the foot), or in the tendon itself behind the ankle bone on the side.
The pain may or may not be accompanied by swelling. It is usually painful or difficult to lift the heel when standing on one leg and to turn the foot inwards when the toes are in a pointed position.
Symptoms tend to be worse with high intensity activity although can be sore day to day when walking or climbing stairs when acute. It is also possible for the foot shape to change, or arch to drop resulting in a flat-foot deformity.
Most tib-post problems can be managed conservatively with Physiotherapy. Physiotherapy may include strengthening exercises for the tendon itself, or for other muscles throughout the leg where there may be a weakness (e.g. gluteal muscles). It may also include calf stretching, taping, ultrasound, soft-tissue work and gait re-education. Advice may be given regarding activity modification, footwear and orthotics. A referral may be made to a Podiatrist for custom-made orthotics.
In the early stage of the tendinopathy, non-steroidal anti-inflammatory medications may be helpful, or a steroid injection around the tendon to calm down any inflammation. There are also many surgical options available if conservative methods fail, some of which are very successful however the post-operative recovery time can be extensive.
A thorough examination comprised of specific questions and physical tests can help to diagnose the cause of your foot or ankle pain. A treatment plan would then be discussed and implemented, to help you towards being pain free and get you back to performing your desired activities. A fundamental part of the treatment plan is explaining the cause of pain and ways to manage it.
Treatment could include hands-on therapy (joint mobilisation/soft tissue massage), a programme of stretches or strength based exercises, Taping, Acupuncture, Ultrasound or perhaps Shockwave Therapy (if appropriate).
If further investigations such as MRI, Ultrasound scan, blood tests or X-rays are required, our Physiotherapists can point you in the right direction. If the Physiotherapist feels you need to see another health professional (such as an Orthopaedic Consultant or Rheumatologist), they will ensure you see the right person via our vast network and close links with consultants.
So, if you have been struggling recently with foot or ankle pain, click here to contact us so we can help you get better!
We usually call you back within the hour during normal working hours
We usually respond within the hour during normal working hours